A Chronic Subdural Hematoma (SDH) is a condition characterized by the accumulation of blood between the outer layer of the brain (dura mater) and the arachnoid membrane. Unlike acute subdural hematomas which develop rapidly after a head injury, chronic SDHs typically evolve over weeks to months. Here are some key points about chronic subdural hematomas:
Causes:
- Head Trauma: Even minor trauma can lead to a chronic SDH, especially in older adults who may have brain atrophy and fragile blood vessels.
- Bleeding Disorders: Conditions that affect blood clotting, such as anticoagulant medications (blood thinners) or clotting disorders, can increase the risk.
- Alcohol Abuse: Chronic alcohol use can weaken blood vessels and increase the risk of bleeding into the subdural space.
- Older Age: The risk of chronic SDH increases with age due to brain atrophy and increased susceptibility to head trauma.
Symptoms:
- Headache: Often dull and persistent.
- Confusion or changes in mental status.
- Nausea and vomiting.
- Weakness or numbness, usually on one side of the body.
- Difficulty Walking or problems with balance.
- Seizures: In some cases, seizures may occur.
Diagnosis:
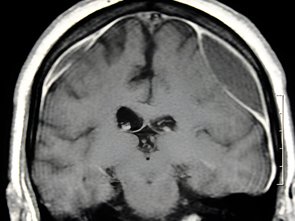
- Imaging: CT (Computed Tomography) scan or MRI (Magnetic Resonance Imaging) of the brain is used to visualize the hematoma and assess its size and location.
- Neurological Examination: Assessment of neurological function to determine the extent of any deficits.
Treatment:
- Observation: Small, asymptomatic chronic SDHs may be monitored closely without immediate intervention.
- Surgical Evacuation: Larger or symptomatic hematomas often require surgical drainage. This procedure involves making a small hole in the skull (burr hole) to drain the collected blood and relieve pressure on the brain. Sometimes, a drain (catheter) may be left in place temporarily to continue draining fluid.
- Medications: In cases where anticoagulant medications are contributing to the bleeding, these may need to be stopped or reversed.
Prognosis:
- With prompt diagnosis and appropriate treatment, many patients recover well after surgical drainage of the hematoma.
- The outcome depends on factors such as the size of the hematoma, the patient’s age and overall health, and any associated neurological deficits.
Complications:
- Recurrence: Chronic SDHs have a risk of recurrence, particularly in elderly patients or those with underlying conditions.
- Brain Injury: Prolonged pressure from a hematoma can lead to permanent brain injury if not treated promptly.
Rehabilitation:
- Physical Therapy: Helps patients regain strength and mobility after surgery.
- Occupational Therapy: Assists with activities of daily living and cognitive rehabilitation.
Management of chronic subdural hematomas requires a multidisciplinary approach involving neurosurgeons, neurologists, and rehabilitation specialists. Early recognition of symptoms and timely intervention are crucial for optimizing outcomes and reducing complications associated with this condition.