Unilateral Biportal Endoscopy of the spine refers to a minimally invasive surgical technique used for accessing and treating spinal disorders. Here’s a breakdown of what this procedure involves:
Technique:
- Minimally Invasive Approach: Biportal endoscopy involves using two small incisions (portals) on one side of the spine. One portal serves as an entry point for the endoscope (a thin, flexible tube with a camera and light source), while the other allows for the insertion of surgical instruments.
- Visualization: The endoscope provides high-definition images of the spinal structures, allowing surgeons to visualize the affected area directly. This is particularly useful for detailed examination of spinal discs, nerves, and surrounding tissues.
- Procedure Flexibility: Unlike traditional open surgery, which requires larger incisions and extensive tissue disruption,Biportal Endoscopy allows for targeted treatment while minimizing trauma to muscles and other soft tissues.
Indications for Use:
- Discectomy: Removal of herniated or degenerated spinal discs causing nerve compression.
- Decompression: Relieving pressure on spinal nerves affected by conditions like spinal stenosis or foraminal stenosis (narrowing of nerve exit openings).
- Facet Joint Treatment: Addressing facet joint arthritis or other conditions affecting these small joints in the spine.
Benefits:
- Minimized Tissue Damage: Preservation of muscle and soft tissue compared to traditional open surgery.
- Faster Recovery: Typically, patients experience less postoperative pain and a quicker return to normal activities.
- Reduced Risk of Complications: Lower risk of infection, blood loss, and other surgical complications.
Considerations:
- Skill and Experience: Biportal Endoscopy requires specialized training and expertise in minimally invasive spine surgery techniques.
- Patient Selection: Not all spinal conditions are suitable for Biportal Endoscopy. The procedure’s applicability depends on the specific diagnosis and the patient’s overall health.
Future Directions:
- Advancing Technology: Continued advancements in endoscopic equipment and techniques may further expand the range of spinal conditions treatable with Biportal Endoscopy.
- Research and Innovation: Ongoing research aims to refine surgical outcomes and broaden the scope of minimally invasive spine surgery options.
In summary, unilateral biportal endoscopy of the spine represents a significant advancement in the field of minimally invasive spine surgery. It offers a tailored approach to treating various spinal disorders while promoting faster recovery and reduced surgical risks. As with any medical procedure, consultation with a qualified spine surgeon is essential to determine the most appropriate treatment approach based on individual circumstances.

Trigeminal Neuralgia (TN) is a chronic pain condition affecting the trigeminal nerve, which is responsible for sensation in the face. This nerve carries sensation from the face to the brain and controls the muscles involved in chewing. Trigeminal Neuralgia is characterized by sudden, severe, and stabbing pain episodes that can be triggered by even mild stimulation of the face, such as brushing teeth, touching the face, or even a breeze.
Key Points about Trigeminal Neuralgia:
- Causes: The exact cause of Trigeminal Neuralgia is often unknown, but it is believed to involve compression or irritation of the trigeminal nerve by a blood vessel, often an artery, near the brainstem. In some cases, it can be caused by multiple sclerosis or a tumor pressing on the nerve.
- Symptoms:
- Episodic Pain: Intense, stabbing, electric shock-like pain in the areas of the face where the branches of the trigeminal nerve are distributed (typically one side of the face).
- Trigger Factors: Pain can be triggered by everyday activities such as eating, talking, brushing teeth, or even a light touch to the face.
- Pain-Free Intervals: Pain episodes may occur in clusters and then have periods of remission.
- Diagnosis:
- Clinical Evaluation: Based on the description of symptoms and triggers.
- Neurological Examination: To assess sensation in the face and rule out other possible causes of facial pain.
- Imaging: MRI of the brain may be performed to rule out structural abnormalities or compression of the trigeminal nerve.
- Treatment:
- Medications:
- Anticonvulsants: Such as carbamazepine (Tegretol), oxcarbazepine (Trileptal), or gabapentin (Neurontin) are commonly used to reduce nerve sensitivity and alleviate pain.
- Muscle Relaxants: Sometimes prescribed to help relax the muscles around the trigeminal nerve.
- Surgical Options:
- Microvascular Decompression (MVD): Surgery to relieve pressure on the trigeminal nerve caused by a blood vessel. This is often considered for patients who do not respond well to medications.
- Gamma Knife Radiosurgery: High-dose radiation directed at the trigeminal nerve root to alleviate pain.
- Balloon Compression or Radiofrequency Thermal Lesioning: Procedures that involve applying heat or pressure to the trigeminal nerve to interrupt pain signals.
- Lifestyle and Home Remedies:
- Avoiding triggers such as cold wind, shaving, or chewing on the affected side.
- Applying heat packs or ice packs to the face during pain episodes.
- Practicing relaxation techniques or biofeedback to manage stress, can exacerbate symptoms.
- Prognosis:
- Trigeminal Neuralgia is a chronic condition that can be challenging to manage, but many individuals find relief with appropriate treatment.
- Some cases may go into remission for long periods, while others may require ongoing management to control symptoms.
Trigeminal Neuralgia can significantly impact daily life due to the unpredictable and intense pain episodes. It’s crucial for individuals experiencing facial pain to seek evaluation and treatment from healthcare professionals experienced in managing this condition, as early intervention can help improve outcomes and quality of life.

Neck Pain is a common problem that can range from mild discomfort to severe, debilitating pain. It can be caused by various factors, including muscle strain, cervical spine disorders, injuries, or underlying health conditions. Here are some common causes and considerations for neck pain:
Common Causes of Neck Pain:
- Muscle Strain: This is often due to poor posture, repetitive movements, or sudden jerking motions that strain the neck muscles.
- Cervical Disk Disorders: Conditions such as herniated disks or degenerative disk disease can cause pain if the disks in the neck are damaged or bulge outward.
- Neck Injuries: Whiplash from a car accident, a fall, or sports injuries can strain the neck muscles and ligaments.
- Joint Disorders: Conditions like osteoarthritis, rheumatoid arthritis, or cervical spondylosis can affect the joints in the neck, causing pain and stiffness.
- Nerve Compression: Herniated disks or bone spurs in the cervical spine can compress nerves, leading to pain, numbness, or weakness that radiates down the arm.
- Poor Posture: Spending long hours hunched over a desk, computer, or smartphone can strain the neck muscles and lead to pain.
- Other Causes: Infections, tumors, or congenital abnormalities can also cause neck pain, although these are less common.
Symptoms Associated with Neck Pain:
- Stiffness: Difficulty moving the neck or turning the head.
- Sharp Pain: Sudden or shooting pain that may radiate down the arm or into the shoulder.
- Headaches: Often originating from tension in the neck muscles.
- Numbness or Tingling: In the arms or hands, indicating nerve involvement.
- Weakness: Difficulty lifting objects or gripping things.
When to See a Doctor:
- Severe Pain: If your neck pain is severe and does not improve with rest or over-the-counter pain relievers.
- Radiating Pain: Pain that radiates down your arms or legs.
- Numbness or Weakness: Especially if it’s affecting your ability to move or use your arms or hands.
- Trauma: If your neck pain follows an injury like a car accident, fall, or blow to the head.
Treatment and Management:
- Rest: Avoid activities that worsen the pain, but gentle movement and stretching can often help relieve stiffness.
- Pain Relief: Over-the-counter pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce inflammation and pain.
- Heat or Ice: Applying heat or ice to the neck can help reduce pain and inflammation. Generally, ice is used in the acute phase (first 48 hours) to reduce swelling, and then heat can be applied to relax muscles.
- Physical Therapy: A physical therapist can teach you exercises to strengthen and stretch the neck muscles, improve posture, and reduce strain.
- Medications: In some cases, muscle relaxants or corticosteroid injections may be prescribed to relieve severe pain or inflammation.
- Surgery:-anterior cervical discectomy and fusion (ACDF), endoscopic cervical discectomy, cervical disc replacement. (CDR).
Prevention:
- Maintain good posture when sitting, standing, and sleeping.
- Take frequent breaks from computer work or other activities that strain the neck.
- Use ergonomic chairs and equipment to support the neck and spine.
- Stay physically active to keep neck muscles strong and flexible.
If you are experiencing persistent or severe neck pain, it’s important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan. They can help determine the underlying cause of your neck pain and recommend the best course of action for relief and recovery.

A Migraine is a neurological condition characterized by recurrent episodes of severe headache, often accompanied by other symptoms such as nausea, vomiting, sensitivity to light, sound, or smells, and sometimes visual disturbances known as auras. Migraine headaches can be debilitating and can last anywhere from a few hours to several days.
There are two main types of migraine:
- Migraine without aura: This is the most common type, where the headache occurs without preceding neurological symptoms (auras).
- Migraine with aura: This type involves specific neurological symptoms that usually precede the headache. These can include visual disturbances (like seeing flashing lights or blind spots), sensory changes (such as tingling sensations in the limbs), or difficulty speaking.
The exact cause of migraines is not fully understood, but they are believed to involve abnormal brain activity affecting nerve signals, blood vessels, and chemicals in the brain. Triggers for migraines can vary widely between individuals and may include stress, hormonal changes, certain foods, lack of sleep, and environmental factors.
Treatment for migraines typically involves managing symptoms during an attack and preventing future episodes. This can include pain-relieving medications (such as NSAIDs or triptans), medications to prevent migraines (such as beta-blockers or antidepressants), lifestyle modifications, and identifying and avoiding triggers.
A Meningioma is a type of tumor that arises from the meninges, which are the layers of tissue covering the brain and spinal cord. These tumors are typically slow-growing and benign (non-cancerous) in most cases.
Types of Meningiomas:
- Benign Meningiomas: The vast majority of meningiomas are benign, meaning they do not invade nearby tissues or spread to other parts of the body.
- Atypical Meningiomas: These tumors have more aggressive features than benign meningiomas but are still considered low-grade.
- Malignant Meningiomas: Rarely, meningiomas can exhibit malignant features and invade nearby tissues or recur after treatment.
Causes and Risk Factors:
- Unknown Cause: The exact cause of meningiomas is often not known.
- Genetic Factors: Some genetic conditions (e.g., neurofibromatosis type 2) increase the risk of developing meningiomas.
Symptoms:
- Variable Symptoms: Depend on the size and location of the tumor.
- Common Symptoms:
- Headaches
- Seizures
- Changes in vision or hearing
- Weakness or numbness in the extremities
- Personality changes or cognitive deficits
Diagnosis:
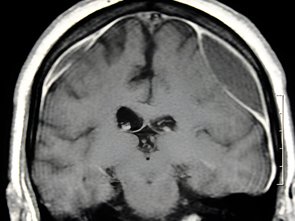
- Imaging: MRI (Magnetic Resonance Imaging) is the preferred imaging modality to visualize meningiomas and assess their size, location, and relation to nearby structures.
- Biopsy: In some cases, a biopsy may be performed to obtain a tissue sample for definitive diagnosis, especially if the MRI findings are inconclusive or suggest a more aggressive tumor.
Treatment Options:
- Observation: Small, asymptomatic meningiomas may be monitored with periodic imaging to assess for growth.
- Surgery: The main treatment for meningiomas involves surgical removal (resection) of the tumor. The goal is to remove as much of the tumor as possible while preserving neurological function.
- Radiation Therapy: Used as an adjuvant treatment after surgery to treat residual tumor or in cases where surgery is not feasible. Techniques include stereotactic radiosurgery (e.g., Gamma Knife) or conventional radiation therapy.
- Medical Therapy: Some meningiomas may express hormone receptors, and hormonal therapy (e.g., somatostatin analogs) may be considered in select cases.
Prognosis:
- Generally Favorable: Benign meningiomas typically have a good prognosis after surgical removal.
- Recurrence: There is a risk of recurrence, especially with atypical or malignant meningiomas.
- Monitoring: Long-term monitoring with periodic imaging is important to detect recurrence or growth.
Management and Follow-Up:
- Multidisciplinary Approach: Treatment planning involves collaboration between neurosurgeons, radiation oncologists, neurologists, and other specialists.
- Supportive Care: Addressing symptoms and providing supportive care to manage any neurological deficits.
Meningiomas are a diverse group of tumors that require individualized treatment based on factors such as tumor size, location, and grade. Advances in imaging, surgical techniques, and radiation therapy have improved outcomes for patients with meningiomas, with an emphasis on preserving neurological function and quality of life.

Low Back Pain is a common issue that many people experience at some point in their lives. It can range from a dull, constant ache to a sudden, sharp sensation that makes movement difficult. Here are some common causes and considerations for low back pain.
- Muscle or Ligament Strain: This is often due to repeated heavy lifting or sudden awkward movements that strain the back muscles and spinal ligaments.
- Bulging or Ruptured Disks: Disks act as cushions between the bones (vertebrae) in your spine. The soft material inside a disk can bulge or rupture and press on a nerve, causing pain.
- Arthritis: different types of arthritis can affect the lower back. In some cases, arthritis in the spine can lead to a narrowing of the space around the spinal cord, a condition called spinal stenosis.
- Skeletal Irregularities: Back pain can occur if your spine curves abnormally. Scoliosis, a condition in which your spine curves to the side, also may lead to back pain, but generally not until middle age.
- Osteoporosis: Your spine’s vertebrae can develop compression fractures if your bones become porous and brittle.
Risk factors: Back pain is more common as you get older, starting around age 30 or 40. Lack of exercise, excessive weight, weight lifting, smoking, and diseases such as arthritis and cancer can increase your risk.
When to see a doctor: Most back pain gradually improves with home treatment and self-care, usually within a few weeks. However, see your doctor if your pain:
- Not subsided with medication and rest
- Associated with sharp shooting leg pain and tingling and numbness of leg
- Difficulty in walking
- Weakness of limb
-
- Causes new bowel or bladder problems
- Is accompanied by fever
- Follows a fall, blow to your back, or other injury
Treatment usually involves staying active and doing exercises to stretch and strengthen your back. Painkillers can help relieve the pain, and in some cases, surgery may be needed. Always consult a healthcare professional for persistent or severe back pain to rule out serious underlying conditions.
When evaluating low back pain, healthcare providers typically follow a systematic approach to identify the cause and determine the appropriate treatment. Here’s a general outline of the workup for low back pain:
- Medical History: The first step is to gather information about your symptoms, how long you’ve had them, any past injuries or conditions related to your back, and any activities or movements that worsen or alleviate the pain.
- Physical Examination.
- Imaging Studies: Depending on the severity and duration of your symptoms, imaging studies may be ordered. These can include:
- X-rays: Useful for evaluating bones and checking for fractures, arthritis, or structural abnormalities.
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues like muscles, ligaments, and disks. It can reveal herniated disks, spinal stenosis, or tumors.
- CT (Computed Tomography) Scan: Sometimes used to get more detailed images of the bones and joints, particularly if a fracture or bone abnormality is suspected.
- Laboratory Tests: Blood tests are not usually necessary for routine low back pain unless there is suspicion of infection, inflammatory conditions, or systemic diseases.
The specific workup may vary depending on individual circumstances and the healthcare provider’s clinical judgment. It’s essential to communicate openly with your healthcare provider about your symptoms, any limitations they cause, and your goals for treatment. This will help guide the diagnostic process and ensure you receive appropriate care for your lower back pain.
Management:-
- Physiotherapy
- Pain Procedure:- Nerve Root Block, Facet Joint Injection
SURGERY:-
- Micro Lumber Discectomy
- Endoscopic Discectomy-trans-foraminal endoscopic discectomy, unilateral-bi portal endoscopic discectomy, PSLD- Percutaneous stenoscopic lumber decompression.
- Micro Lumber Decompression Plus Fixation
- TLIF (Transforaminal Lumber Interbody Fusion)
- MIS TLIF (Minimally Invasive Spine Surgery)
- OLIF (Oblique Lumber Interbody Fusion)
- MIS Fixation
- Kyphoplasty
- Vertebroplasty

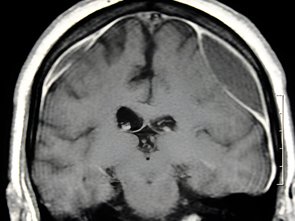
Hydrocephalus is a condition characterized by an abnormal accumulation of cerebrospinal fluid (CSF) within the cavities (ventricles) of the brain. This buildup of fluid can increase pressure inside the skull, leading to potentially serious symptoms and complications. Here are some key points about hydrocephalus:
Causes:
- Obstruction: Most cases are caused by a blockage that prevents proper drainage of CSF. This obstruction can occur due to congenital factors (present at birth) such as developmental abnormalities or aqueductal stenosis (narrowing of a passage in the brain).
- Impaired Absorption: Sometimes, hydrocephalus can result from problems with CSF absorption in the brain. This can be due to infections, hemorrhages, or certain tumors affecting the structures that normally reabsorb CSF.
- Secondary Causes: Hydrocephalus can also develop as a secondary condition following head injuries, strokes, infections (such as meningitis), or tumors that interfere with CSF circulation.
Types of Hydrocephalus:
- Congenital Hydrocephalus: Present at birth, often due to developmental abnormalities or genetic factors.
- Acquired Hydrocephalus: Develops after birth due to trauma, infection, tumors, or other medical conditions affecting the brain.
- Normal Pressure Hydrocephalus (NPH): Characterized by a gradual onset of symptoms in older adults. Unlike other types, NPH may not always present with increased pressure inside the skull.
Symptoms:
- Infants and Children: Rapid increase in head circumference, bulging fontanelles (soft spots), vomiting, irritability, seizures, and developmental delays.
- Adults: Headache, nausea, vomiting, cognitive difficulties (memory loss, impaired concentration), gait disturbances (difficulty walking), urinary incontinence, and vision changes.
Diagnosis:
- Imaging: CT scan or MRI of the brain to visualize the ventricles and assess the extent of fluid accumulation.
- Monitoring Pressure: In some cases, monitoring intracranial pressure may be necessary to assess the severity of hydrocephalus.
Treatment:
- Surgical Options:
- Shunt Placement: The most common treatment involves surgically placing a shunt system to divert excess CSF from the brain to another part of the body (such as the abdomen) where it can be absorbed.
- Endoscopic Third Ventriculostomy (ETV): An alternative procedure that creates a new pathway for CSF drainage within the brain, bypassing the blockage.
- Medications: Sometimes, medications may be used to reduce CSF production or to manage symptoms associated with hydrocephalus.
Prognosis:
- With prompt diagnosis and appropriate treatment, many individuals with hydrocephalus can lead normal lives.
- Long-term management and monitoring are often necessary, as complications such as shunt malfunction or infection can occur.
Support and Care:
- Regular follow-up visits with healthcare providers are essential to monitor for complications and adjust treatment as needed.
- Support groups and resources can provide valuable information and emotional support for individuals and families affected by hydrocephalus.
Hydrocephalus is a complex condition that requires specialized care. If you suspect you or someone else may have symptoms of hydrocephalus, it’s important to seek medical attention promptly for proper evaluation and management.

Hemifacial Spasm is a neuromuscular disorder characterized by involuntary contractions or twitching of the muscles on one side of the face. This condition typically begins with twitching around the eye and can gradually progress to involve other muscles on the affected side of the face, including the cheek, mouth, and neck.
Key Points about Hemifacial Spasm:
- Causes:
- Compression of Facial Nerve: The most common cause is compression of the facial nerve (cranial nerve VII) by a blood vessel, usually an artery, near the brainstem. This compression leads to abnormal signals being sent to the facial muscles, causing them to twitch involuntarily.
- Idiopathic: In some cases, no clear cause can be identified, and the condition is termed idiopathic hemifacial spasm.
- Symptoms:
- Involuntary Muscle Twitching: Typically begins around the eye (eyelid twitching) and may progress to involve other muscles on one side of the face.
- Continuous or Intermittent: Twitching can be continuous or intermittent and may worsen with stress, fatigue, or certain movements of the face.
- No Sensory Loss: Unlike conditions affecting the trigeminal nerve, there is no loss of sensation in the affected area.
- Diagnosis:
- Clinical Evaluation: Based on the history and description of symptoms.
- Neurological Examination: To assess the extent and pattern of muscle involvement.
- Electromyography (EMG): Used to detect abnormal electrical activity in the facial muscles, confirming the diagnosis.
- Treatment:
- Botulinum Toxin Injections: Botulinum toxin (Botox) injections are the primary treatment for hemifacial spasms. The toxin temporarily paralyzes the facial muscles, reducing involuntary movements.
- Medications: Anticonvulsant medications such as carbamazepine or antispasmodic drugs may provide partial relief in some cases.
- Surgical Options:
- Microvascular Decompression (MVD): Similar to the treatment for trigeminal neuralgia, MVD surgery involves placing a cushion (usually Teflon).
A Chronic Subdural Hematoma (SDH) is a condition characterized by the accumulation of blood between the outer layer of the brain (dura mater) and the arachnoid membrane. Unlike acute subdural hematomas which develop rapidly after a head injury, chronic SDHs typically evolve over weeks to months. Here are some key points about chronic subdural hematomas:
Causes:
- Head Trauma: Even minor trauma can lead to a chronic SDH, especially in older adults who may have brain atrophy and fragile blood vessels.
- Bleeding Disorders: Conditions that affect blood clotting, such as anticoagulant medications (blood thinners) or clotting disorders, can increase the risk.
- Alcohol Abuse: Chronic alcohol use can weaken blood vessels and increase the risk of bleeding into the subdural space.
- Older Age: The risk of chronic SDH increases with age due to brain atrophy and increased susceptibility to head trauma.
Symptoms:
- Headache: Often dull and persistent.
- Confusion or changes in mental status.
- Nausea and vomiting.
- Weakness or numbness, usually on one side of the body.
- Difficulty Walking or problems with balance.
- Seizures: In some cases, seizures may occur.
Diagnosis:
- Imaging: CT (Computed Tomography) scan or MRI (Magnetic Resonance Imaging) of the brain is used to visualize the hematoma and assess its size and location.
- Neurological Examination: Assessment of neurological function to determine the extent of any deficits.
Treatment:
- Observation: Small, asymptomatic chronic SDHs may be monitored closely without immediate intervention.
- Surgical Evacuation: Larger or symptomatic hematomas often require surgical drainage. This procedure involves making a small hole in the skull (burr hole) to drain the collected blood and relieve pressure on the brain. Sometimes, a drain (catheter) may be left in place temporarily to continue draining fluid.
- Medications: In cases where anticoagulant medications are contributing to the bleeding, these may need to be stopped or reversed.
Prognosis:
- With prompt diagnosis and appropriate treatment, many patients recover well after surgical drainage of the hematoma.
- The outcome depends on factors such as the size of the hematoma, the patient’s age and overall health, and any associated neurological deficits.
Complications:
- Recurrence: Chronic SDHs have a risk of recurrence, particularly in elderly patients or those with underlying conditions.
- Brain Injury: Prolonged pressure from a hematoma can lead to permanent brain injury if not treated promptly.
Rehabilitation:
- Physical Therapy: Helps patients regain strength and mobility after surgery.
- Occupational Therapy: Assists with activities of daily living and cognitive rehabilitation.
Management of chronic subdural hematomas requires a multidisciplinary approach involving neurosurgeons, neurologists, and rehabilitation specialists. Early recognition of symptoms and timely intervention are crucial for optimizing outcomes and reducing complications associated with this condition.

Atlantoaxial Dislocation refers to an abnormal alignment or displacement of the first (atlas) and second (axis) cervical vertebrae in relation to each other. This condition can lead to compression or instability of the spinal cord or spinal nerves in the upper cervical spine. Here’s a detailed overview:
Anatomy and Function:
- Atlas (C1): The first cervical vertebra that supports the skull and allows for nodding movements of the head.
- Axis (C2): The second cervical vertebra that allows rotational movements of the head.
Causes of Atlantoaxial Dislocation:
- Congenital Anomalies: Abnormalities in the development of the vertebrae or ligaments.
- Trauma: Injury to the cervical spine, such as fractures or ligamentous injuries, can lead to instability.
- Connective Tissue Disorders: Conditions like Down syndrome or Ehlers-Danlos syndrome can predispose individuals to atlantoaxial instability.
- Inflammatory Conditions: Rheumatoid arthritis or other inflammatory diseases affecting the cervical spine.
Symptoms:
- Neck Pain: Often localized at the base of the skull or upper neck.
- Headaches: Especially worsened by movement.
- Neurological Symptoms: Depending on the severity and compression of spinal structures, symptoms can include weakness, numbness, or tingling in the arms or legs.
- Difficulty Walking: In severe cases, due to spinal cord compression.
- Bowel or Bladder Dysfunction: Rarely, in cases of severe spinal cord compression.
Diagnosis:
- Imaging: MRI and CT scans of the cervical spine to visualize the alignment of the vertebrae, assess for spinal cord compression, and identify any associated abnormalities.
- Dynamic Imaging: X-rays or MRI with flexion-extension views to evaluate for instability during different head and neck positions.
Treatment Options:
- Conservative Management: In mild cases or when surgery is not feasible, treatment may involve immobilization with a cervical collar and close monitoring.
- Surgical Intervention: Often required for symptomatic or severe cases to stabilize the spine and decompress neural structures. Surgical options may include:
- Posterior Cervical Fusion: Using bone grafts and metal hardware to fuse the affected vertebrae.c1-c2 fixation , occipito cervical fixation.
- Instrumentation: Placement of screws and rods to stabilize the spine.
- Transoral Odontoidectomy: Surgical removal of the top of the axis vertebra to relieve compression in specific cases.
- Physical Therapy: Rehabilitation to improve neck strength and range of motion, and to help restore function post-surgery.
Prognosis:
- The prognosis depends on the underlying cause, severity of dislocation, and timely intervention.
- Early diagnosis and appropriate treatment can lead to good outcomes in many cases, especially when neurological symptoms are minimal or absent.
Complications:
- Without treatment, atlantoaxial dislocation can lead to progressive neurological deficits, spinal cord injury, or even paralysis in severe cases.
Management Approach:
- Management typically involves a multidisciplinary team including neurosurgeons, and rehabilitation therapists to tailor treatment plans to individual needs.
Atlantoaxial Dislocation is a complex condition that requires careful evaluation and treatment planning to address spinal stability and prevent neurological complications. Individuals experiencing symptoms suggestive of cervical spine instability should seek evaluation by a healthcare provider experienced in managing spinal disorders.

Symptoms:-
- Neck pain
- Tingling numbness
- Pain around the shoulder blade
- Pain along the arm and in the fingers
- Increasing pain during standing, sitting, sneezing, coughing, or bending the neck backward
- Muscle weakness, making it difficult to lift the arm or grasp things
- Stiffness
- Headaches, mostly in the back of the head
- Numbness or tingling sensation in the shoulder and arms
- Loss of balance and control over bladder and bowel movements
Management Options:-
Investigation
- Clinical Assessment
- Xray Cervical Spine
- MRI
Conservative Trial (medicine, physiotherapy, postural modification)
Surgical:-
- Anterior cervical discectomy and fusion
- Anterior cervical corpectomy with fusion
Cervical Compressive Myelopathy:-
- Neck pain
- Tingling numbness
- Pain around the shoulder blade
- Tightness of all 4 limbs
- Difficulty in walking
- Pain along the arm and in the fingers
- Muscle weakness, making it difficult to lift the arm or grasp things
- Neck pain and stiffness
- Headaches, mostly in the back of the head
- Numbness or tingling sensation in the shoulder and arms
- Loss of balance and control over bladder and bowel movements
Causes:-
- Ossified posterior longitudinal ligament
- Cervical canal stenosis
Management Options:-
Investigation
- Clinical Assessment
- Xray Cervical Spine
- MRI
Conservative Trial (medicine, physiotherapy, postural modification)
Surgical:-
- Anterior cervical approach
- Posterior cervical approach- cervical laminectomy and lateral mass fixation
Lumber Disc Problem:-
- Back Pain
- Tingling Numbness
- Lower limb Weakness
- Bowel Bladder Deficit
- Sensory Deficit
Management options:-
Investigation
- Conservative Trial
- Micro Lumber Discectomy
Surgical:-
- Endoscopic discectomy, trans-foraminal endoscopic discectomy, unilateral-bi portal endoscopic discectomy, PSLD-Percutaneous Stenoscopic Lumber Decompression
Lumber Canal Stenosis:-
- Back pain
- Tingling numbness in the lower limb
- Unable to stand
- Difficulty in walking due to severe pain
- Lower limb Weakness
- Bowel bladder deficit
- Sensory deficit
Management Options:-
Investigation
- MRI
- Xray:-Dynamic x-ray LS spine
- Conservative Trial
Surgical:-
- Micro lumber decompression plus fixation
- TLIF (Transforaminal Lumber Interbody Fusion)
- MIS TLIF (Minimally Invasive Spine Surgery)
- OLIF (Oblique Lumber Interbody Fusion)
- MIS FIXATION
- MIS TLIF
- OLIF
Neutral Tube Defect:-
- Swelling at back
- Limb weakness
- Bowel bladder incontinence
- Sensory deficit
- Non-healing ulcer
- Associated with hydrocephalus
- Neuro-cutaneous marker
- Discharging sinus from the back
Management Option:-
- Headache
- Altered sensorium
- Multiple episodes of vomiting
- Convulsion
- Visual disturbances
- Limb weakness
- Vertigo
- Hearing loss
- Difficulty in speaking
- Voice changes
Early Treatment, Gives Good Results, Increases Life Survival
- Falcine meningioma
- Glioblastoma multiformis
- Sellar Suprasellar SOL
Management:-

Lumbar Disk Disease affects the lower back region, which is home to the five bone segments that altogether make up the lumbar spine.
How Does Lumbar Disk Disease Occur?
Modifying the normal disk’s structure is the root reason for lumbar disk disease. Lumbar Disk disease typically at times results from aging and the regular breakdown that takes place within the disk. Severe trauma can occasionally result in a normal disk herniating. An already-existing herniated disk may deteriorate due to injuries as well.
What Are the Chances Of Developing a Lumbar Disk Disease?
Physical inactivity can result in weak back and abdominal muscles, which may not support the spine effectively, even though age is the most common risk factor in this case. Additionally, the prevalence of back problems increases in cases that are typically inactive but suddenly active and participate in overly strenuous activities. Jobs that require twisting or maybe heavy lifting of the spine can even cause back injuries.
For accurate knowledge and rapid cure talk to the Best Spine Surgeon In the North-East!

The long-term, severe mental illness known as Schizophrenia alters a person’s opinions, behavior, emotional expression, reality perception, and interpersonal relationships. Schizophrenia isn’t as common as the other severe mental illnesses but it is one of the most chronic and disabling.
Schizophrenia patients frequently struggle in relationships, their workplace, the classroom, and society at large. They could have lost contact with reality, felt afraid, and withdrawn. Although there is no remedy at all for this incurable illness, it can be managed to some extent with the right care.
Schizophrenia is not at all a multiple or split personality, despite common perception. Psychosis—a form of mental illness in which an individual is unable to differentiate between what is imagined and what is real—is an element of schizophrenia.
For more information, talk to the Best Neurosurgeon In the North-East!
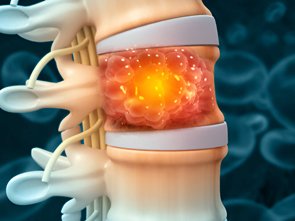
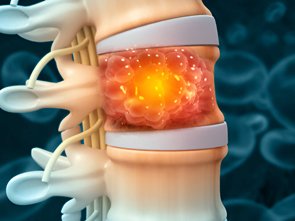
A Spine Tumor refers to an abnormal growth of cells within or near the spinal column. These tumors can be either primary (originating in the spine) or secondary (metastatic tumors spreading to the spine from other parts of the body). Here’s an overview of spine tumors, including their types, symptoms, diagnosis, and treatment:
Types of Spine Tumors:
- Primary Spine Tumors:
- Intramedullary Tumors: Arise from within the spinal cord itself, such as ependymomas or astrocytomas.
- Intradural-Extramedullary Tumors: Develop within the dura (covering of the spinal cord) but outside the spinal cord, like meningiomas or nerve sheath tumors (schwannomas).
- Extradural Tumors: Originate from structures outside the spinal cord and dura, often involving bones or nearby tissues. Examples include metastatic tumors (from breast, lung, prostate, etc.), chordomas, or osteosarcomas.
- Metastatic Spine Tumors: These are the most common spine tumors and originate from cancers that have spread (metastasized) to the spine from other parts of the body, such as the lungs, breasts, or prostate.
Symptoms:
- Back Pain: Persistent and often worsens at night or with activity.
- Neurological Deficits: Weakness, numbness, or tingling in the limbs.
- Difficulty Walking: Due to compression of spinal nerves or spinal cord.
- Loss of Bowel or Bladder Control: In severe cases, due to spinal cord compression.
Diagnosis:
- Imaging: CT scan or MRI of the spine to visualize the tumor’s location, size, and extent of involvement.
- Biopsy: Removal of a small sample of the tumor tissue for examination under a microscope to determine the type of tumor and its aggressiveness.
Treatment Options:
- Surgery: Often the mainstay of treatment for spine tumors, aiming to remove as much of the tumor as possible while preserving spinal stability and function. Techniques may include minimally invasive procedures or extensive spinal reconstruction, depending on the tumor’s location and size.
- Radiation Therapy: Used to shrink tumors, relieve symptoms, or as adjuvant therapy after surgery to destroy remaining cancer cells.
- Chemotherapy: Typically used for certain types of primary spine tumors or metastatic tumors that are sensitive to chemotherapy drugs.
- Targeted Therapy: Drugs that specifically target molecular changes in tumor cells may be used in certain types of spine tumors.
- Pain Management: Medications, physical therapy, and interventional procedures (such as nerve blocks or spinal cord stimulators) may be used to manage pain associated with spine tumors.
Prognosis:
- The outlook varies widely depending on the type of tumor, its location, the extent of spread, and the patient’s overall health.
- Metastatic spine tumors generally have a poorer prognosis compared to primary spine tumors.
Rehabilitation:
- Physical therapy and rehabilitation play a crucial role in restoring mobility, strength, and function after spine tumor treatment, especially surgery.
Multidisciplinary Approach:
- Management of spine tumors often involves a team of specialists, including neurosurgeons, oncologists, radiation oncologists, and rehabilitation therapists, to provide comprehensive care tailored to each patient’s needs.
Early diagnosis and prompt treatment are essential for optimizing outcomes and quality of life for individuals with spine tumors. Regular follow-up care is important to monitor for any signs of recurrence or complications.
For knowledge and rapid cure talk to the Best Spine Surgeon In Coochbehar!

Loss of thinking ability, memory, attention, logical reasoning, and other mental abilities is referred to and comes under a broad term – Dementia, a general phrase. These alterations are substantial enough to cause problems with social or professional functioning.
Dementia can be brought on by a variety of factors. It occurs when there is illness or damage to the areas of the brain responsible for language, learning, memory, and decision-making. It may also be referred to as a significant neurocognitive disorder. But it is not an illness. Rather, it’s a collection of signs brought on by different illnesses.
A percentage of 5% to 8% of persons over 65 suffer from dementia. After 65, this percentage doubles every five years. Up to 50% of adults in their 80s suffer from dementia.
Alzheimer’s disease most commonly causes dementia.
To get enlightened, talk to the Best Neurosurgeon In Coochbehar!

Epilepsy is a neurological disorder characterized by recurrent seizures, which are sudden, brief changes in the brain’s electrical activity. These seizures can cause a wide range of symptoms, from brief lapses in consciousness to violent muscle spasms. Here are some key points about epilepsy:
Types of Seizures:
- Generalized Seizures:
- Tonic-Clonic (Grand Mal) Seizures: Involves loss of consciousness, and stiffening of muscles (tonic phase), followed by rhythmic jerking (clonic phase).
- Absence Seizures: Brief loss of awareness or “staring spells,” more common in children.
- Myoclonic Seizures: Sudden, brief muscle jerks or twitches.
- Focal (Partial) Seizures:
- Simple Focal Seizures: May cause twitching or a change in sensation without loss of consciousness.
- Complex Focal Seizures: Alters consciousness and may cause repetitive movements like chewing or hand rubbing.
Causes:
- Idiopathic: No identifiable cause; likely due to genetic factors.
- Symptomatic: Result from brain injury (such as head trauma), stroke, brain tumors, infections (like meningitis), or developmental disorders (like cerebral palsy).
Diagnosis:
- Medical History: Detailed description of seizure episodes and their characteristics.
- Electroencephalogram (EEG): Records the brain’s electrical activity and helps classify seizure types.
- Imaging: MRI or CT scans to identify structural abnormalities or lesions in the brain.
Treatment:
- Medications (Antiepileptic Drugs – AEDs):
- Prescribed based on seizure type and individual response.
- Examples include carbamazepine, valproic acid, lamotrigine, and levetiracetam.
- Surgery:
- It is considered for some individuals with epilepsy that don’t respond to medications.
- Options include removing the area of the brain causing seizures or implanting devices to help control seizures.
- Vagus Nerve Stimulation (VNS):
- Involves implanting a device that sends electrical impulses to the vagus nerve, which may help reduce seizure frequency.
- Ketogenic Diet:
- High-fat, low-carbohydrate diet may reduce seizures in some children and adults with epilepsy.
Management and Lifestyle:
- Seizure Action Plan: Develop a plan with healthcare providers to manage seizures effectively.
- Regular Medical Care: Monitor medication levels, side effects, and overall health.
- Lifestyle Modifications: Ensure adequate sleep, manage stress, and avoid triggers like alcohol or specific foods.
Prognosis:
- Varies Widely: Depends on seizure type, cause, response to treatment, and individual factors.
- Many People Manage Well: With medications or other treatments, most individuals with epilepsy can lead normal lives.
Support and Resources:
- Epilepsy Foundation and other organizations provide support, education, and resources for individuals and families affected by epilepsy.
Managing epilepsy involves a collaborative approach between healthcare providers, patients, and caregivers to find the most effective treatment plan tailored to each individual’s needs. Regular follow-up and adherence to treatment recommendations are crucial for optimizing seizure control and quality of life
For treatment, talk to the Best Neurosurgeon In Coochbehar and get instantaneous results!

Most people are unaware of how complicated headaches may be. There are several types of headaches and each one has its distinct reasons. Knowing what kind of headache one has can help the individual and the doctor determine the best course of action, including making an effort to prevent further headaches.
Typical Headache Types
Over 150 different kinds of headaches exist, but the following are the most prevalent ones:
- Tension Headaches
- Migraine Headaches
- Cluster Headaches
- Chronic Daily Headaches
- Sinus Headaches
- Posttraumatic Headaches
A few months may pass between headaches. But it is important at the same time to talk to the Best Neurosurgeon In the North-East, after a few weeks, if it doesn’t tend to improve.

A Cerebrovascular Accident (CVA), commonly known as a stroke, occurs when there is a disruption in the blood supply to the brain, resulting in damage to brain tissue. Strokes can be broadly categorized into two main types:
- Ischemic Stroke: This is the most common type, accounting for about 85% of all strokes. It occurs when a blood clot or atherosclerotic plaque blocks or narrows an artery leading to the brain. As a result, the affected part of the brain does not receive enough oxygen and nutrients, leading to tissue damage.
- Hemorrhagic Stroke: This type occurs when a blood vessel in the brain bursts or leaks. This bleeding puts pressure on brain tissue and can damage cells. Hemorrhagic strokes can result from conditions such as high blood pressure (hypertension), aneurysms, arteriovenous malformations (AVMs), or head trauma.
Who Is Impacted By It?
All ages can undergo a stroke, including children and adults, but again some individuals have a greater risk and are more vulnerable than others. Strokes are also more familiar in the later age (those over 65 account for around two-thirds of all stroke cases).
Also, some medical disorders, such as high blood pressure (hypertension), high cholesterol (hyperlipidemia), Type 2 diabetes, and those with a history of stroke, and heart attack increase the threat of stroke!
Symptoms of Stroke:
- Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body.
- Sudden confusion, trouble speaking, or difficulty understanding speech.
- Sudden trouble seeing in one or both eyes.
- Sudden severe headache with no known cause.
- Sudden trouble walking, dizziness, loss of balance, or coordination.
Diagnosis:
- Physical Examination: A healthcare provider will assess symptoms, neurological function, and vital signs.
- Imaging Tests: CT (Computed Tomography) scan or MRI (Magnetic Resonance Imaging) is used to visualize the brain and determine the type and location of the stroke.
- Blood Tests: These may be done to check blood sugar levels, electrolytes, and to rule out other possible causes of symptoms.
Treatment:
- Ischemic Stroke: Immediate treatment often involves dissolving or removing the clot to restore blood flow to the brain. This can be done with clot-busting medications (like tissue plasminogen activator – tPA) or mechanical thrombectomy (surgical removal of the clot).
- Hemorrhagic Stroke: Treatment aims to control bleeding, reduce pressure on the brain, and stabilize vital signs. Surgery may be necessary to repair blood vessel abnormalities or to remove blood from the brain.
Rehabilitation:
- After the acute phase of treatment, rehabilitation plays a crucial role in stroke recovery. Physical therapy, speech therapy, occupational therapy, and lifestyle modifications are often part of a comprehensive rehabilitation program.
Prevention:
- Risk Factor Management: Controlling high blood pressure, managing diabetes, quitting smoking, and maintaining a healthy diet and weight are important preventive measures.
- Medications: Aspirin or other antiplatelet medications may be recommended to reduce the risk of ischemic stroke in certain individuals.
Prompt recognition of stroke symptoms and quick medical intervention are critical for minimizing brain damage and improving outcomes. If you or someone else experiences symptoms of a stroke, it is essential to seek emergency medical attention immediately.
For consultation and greater knowledge talk to the Best Neurosurgeon In Coochbehar and get relieved instantaneously!

Parkinson’s disease is a neurological condition that progresses over time and affects a small portion of neurons in the substantia nigra, an area of the brain. Dopamine is a chemical substance (neurotransmitter) that is regularly produced by these cells. When the brain functions normally, it transfers messages between different locations that coordinate smooth, balanced muscular activity. Movements of the body are altered when these nerve cells die, which is what happens in Parkinson’s disease.
What Are the Signs Of Parkinson’s Disease?
Typical signs of Parkinson’s Disease consists of:
- Stiffness Of Muscles
- Shivers
- Bradykinesia – characterized by a slowdown in movement and a progressive lack of spontaneous activity.
- Changes in posture and walking manner
- Changes in handwriting and speech
- Imbalance and a rise in falls
- Orthostatic hypotension – a decrease in blood pressure when standing resulting in fainting
For more, talk to the Best Neurosurgeon In the North-East!